STORY #3
Preventing sarcopenia
which leads to lower QOL
Kiyoshi Sanada, Ph.D.
Professor, College of Sport and Health Science
Sarcopenia and obesity,
clarifying its mortality risk
Starting April 2020, Japan initiated a program known as Fureiru Kenshin (frailty screening) for those over 75 years of age. In response, Ritsumeikan University released a video by Kiyoshi Sanada, who has vast research experience in related fields, explaining how to take measures against frailty and the importance of taking these measures.
The term Fureiru comes from the English word frail. “In this context, frail, or frailty points to the declining conditions of the physical, mental, emotional and social aspects of one’s self as a whole,” Sanada explains. In Japan, as it crosses the threshold of an ultra-aged society, attention on frailty has been on the rise; it is now increasingly perceived as a percurrent stage before the older adults come to require care. Sarcopenia is given particular attention as one of the contributing factors to the physical aspects of frailty. Thus far, Sanada has focused on sarcopenia and poured his energy and time into researching what could lead to its preventative measures.
Sarcopenia refers to the severe loss of muscle mass due to aging, which leads to highly diminished muscle strength. Typically, this process begins more or less at the age of 40 in men and at about the age of 35 in women. “When the decline of muscles is combined with other issues, the risk of contracting lifestyle diseases such as osteoporosis and diabetes starts to rise, and quality of life (QOL) starts to decline rapidly,” says Sanada, while explaining the dangers of sarcopenia.
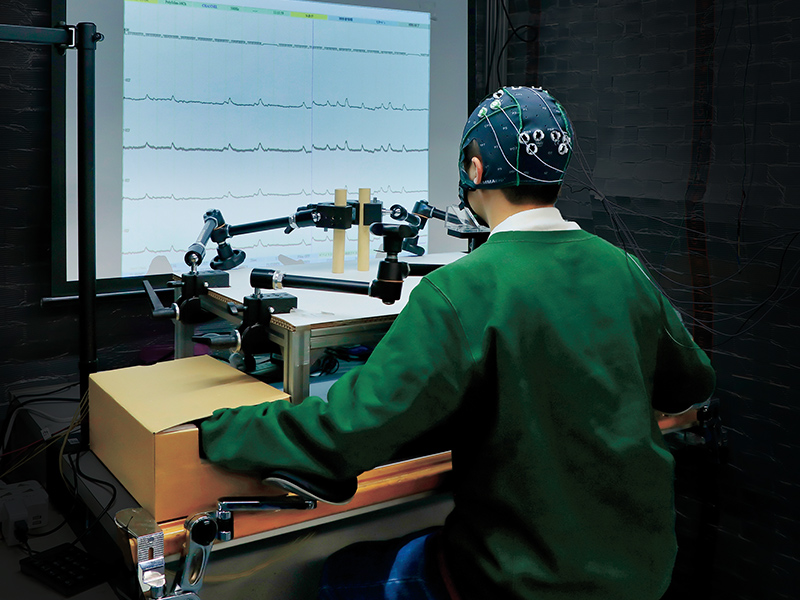
Having realized the importance of this issue, Sanada has long engaged in establishing standards for evaluating and diagnosing sarcopenia in Japan. “When I started, a European research group had defined standard values to determine whether somebody had sarcopenia using dual-energy X-ray absorptiometry (DXA). The DXA method is widely known for determining muscle and bone mass. However, Western and Asian people typically have different physical structures than each other. So, it didn’t seem appropriate to apply those European standards to the Japanese context. This is why I thought it necessary to come up with a diagnostic standard for evaluating sarcopenia in Japanese people,” Sanada explains, while elucidating his motivation behind his research. To achieve this first research goal, he describes, Sanada conducted a large-scale study involving physical examinations of over 1,800 Japanese men and women between the ages of 18 and 85, including body composition measurements using the DXA method and data from simplified physical fitness tests, to calculate values that could be set as the sarcopenia evaluation standards for Japanese people.
Among his assessments, first was the SMI (skeletal muscle index), which is calculated by determining the height2-adjusted appendicular muscle mass index. According to this formula, the SMI values for subjects under the age of 40 were 8.67±0.9 kg/m2 for men and 6.78±0.66 kg/m2 for women. Based on previous study, Sanada set a standard deviation of -2 from the mean value of the subjects’ SMI as the reference for sarcopenia in the Japanese population. He considered a standard deviation of -1 from SMI’s mean value as the pre-sarcopenia category. Plugging these numbers into the formula, he calculated the reference values for sarcopenia to be 6.78 for men and 5.46 for women. Reference values for pre-sarcopenia were calculated to be 7.77 for men and 6.12 for women.
However, while calculations using the DXA method are quite precise, measurements for the calculation cannot be easily taken. For this reason, Sanada also developed a simple evaluation method for sarcopenia based on age, BMI, waist circumference, grip strength, and the size of the calf. But how could all of this advanced research be applied to society to benefit the people? Sanada’s primary focus has remained on answering this question.
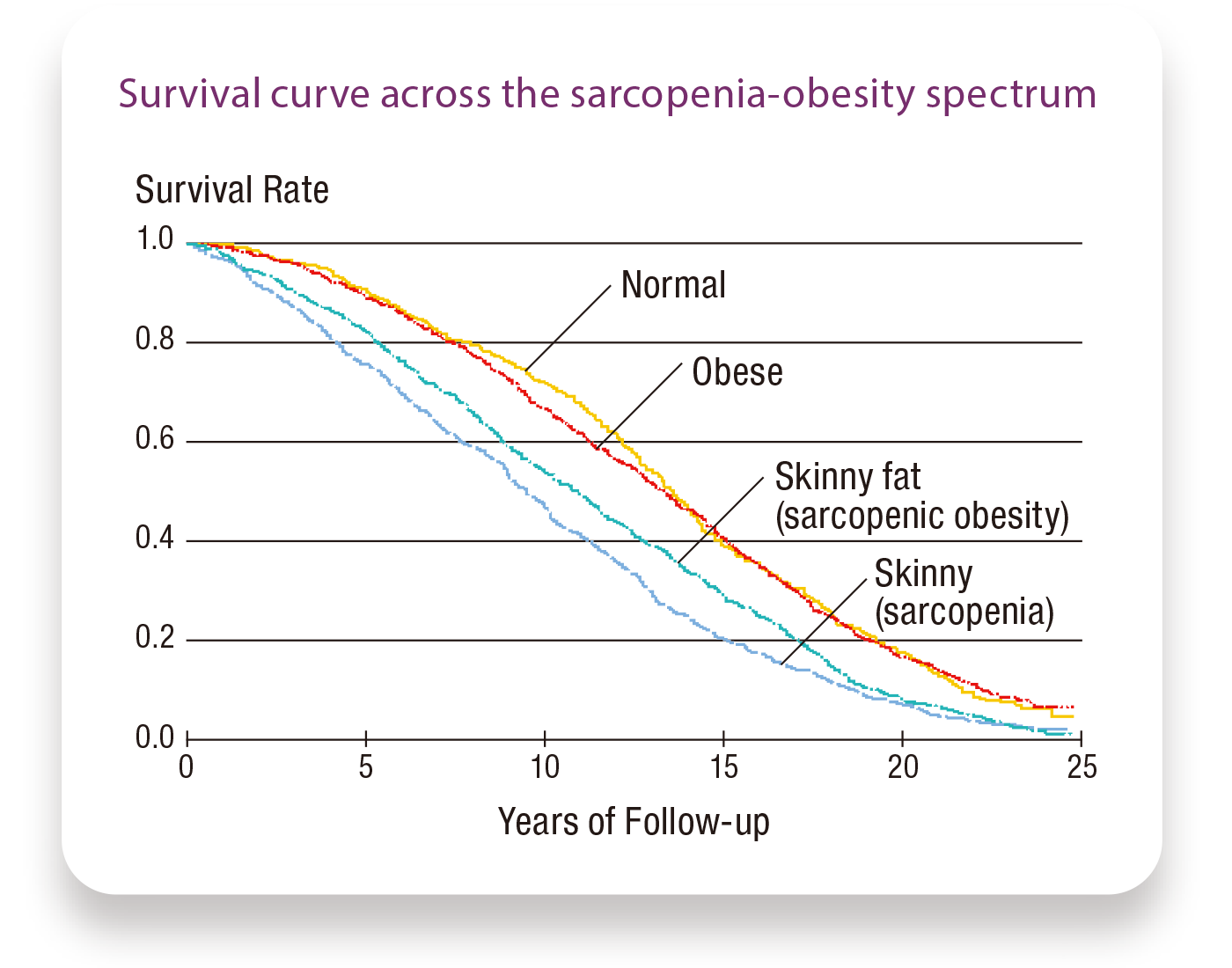
Further, through his joint research with the University of Hawaii, Sanada got some interesting insights into the relationship between sarcopenic obesity and mortality risk. “Using cohorts from an over 50-year old (since 1965) epidemiological study of Japanese-Americans in Hawaii, mortality data were available for up to 24 y of follow-up, from 1991 to 2015, corresponding to approximately 2,300 Japanese-American men. Using that data, I examined the relationship between sarcopenia and obesity and their combined relation to mortality risk,” he says.
To perform the data analysis, Sanada divided the subjects into four categories based on their body types: normal, obese, skinny (sarcopenia), and skinny fat (sarcopenic obesity). Then he calculated the mortality risk for each type. “In our hypothesis, we thought that those with sarcopenic obesity—meaning those who are obese and experiencing sarcopenia simultaneously—would have the highest mortality risk. However, contrary to our expectations, those who were skinny, that is, those with sarcopenia but no obesity, had the highest mortality risk,” says Sanada. Why was this the case?
Sanada came up with an answer. According to him, what we need to be focusing on is the subject’s age. “The research material we used was that of a cohort with very advanced ages. The average age of the subjects was 78. From about 75 years of age, a phenomenon known as the obesity paradox begins to occur. That is to say, after you turn 75, the older you get, the more importance your body fat gains. Our study seemed to indicate this phenomenon as well,” Sanada analyzes. He further states that we should be paying attention to the high mortality risk of sarcopenia. “We should not forget that after the age of 40, the stage of life that immediately precedes becoming an advanced elderly, obesity is a serious risk factor. This is one of the reasons that we should start taking preventative measures early,” Sanada emphasizes.
Countermeasures taken against sarcopenia also work towards frailty prevention. For this reason, Sanada’s research interest expanded to include frailty. He used evaluation metrics to verify the state of frailty amongst the Japanese population, conducting frailty tests on the general public living in Koka city, Shiga prefecture, while raising awareness for frailty prevention.
Based on his research, Sanada thinks that when frailty-related conditions and obesity are simultaneously present, ADL (activities of daily living) indices, sarcopenia, and locomotive syndrome, among others, would worsen as well. “Most recent reports have stated that when frail people catch the novel coronavirus, the mortality rate increases,” explains Sanada, highlighting how the importance of his research is becoming even more pronounced.
A video explaining how to take measures against frailty

- Kiyoshi Sanada, Ph.D.
- Professor, College of Sport and Health Science
- Specialties: Exercise physiology, applied health science
- Research Themes: Constructing scientific evidence towards the development of exercise prescription to prevent lifestyle-related diseases; how obesity-related genes, amount of physical activity, and food intake conditions affect the development of metabolic syndrome; the development of evaluation criteria and simple evaluation methods for sarcopenia or sarcopenic obesity in adult Japanese men and women.